Breast cancer is not terrifying! As long as it is detected early and treated appropriately, the 5-year survival rate at stage I can reach 99%, while at stage IV it drops to around 30%.
Early-stage breast cancer often has no symptoms. Data from the Hong Kong Breast Cancer Foundation shows that over 90% of patients present with a painless lump, but self-examination may not always detect it, making regular screening essential.
Currently, breast imaging options include Breast Magnetic Resonance Imaging (MRI), Mammography, and Breast Ultrasound. Both MRI and mammography can detect non-palpable lumps and early microcalcifications, aiding in the early diagnosis of stage I breast cancer. Among them, breast MRI has higher sensitivity—over 90%—and is particularly suitable for high-risk women and those aged 40 or above concerned about breast health.
Since breast characteristics and risk factors differ by age, choosing the right screening method improves accuracy. Below are recommendations for women in their 20s, 30s, and 40s.
Question 1: What is breast cancer?
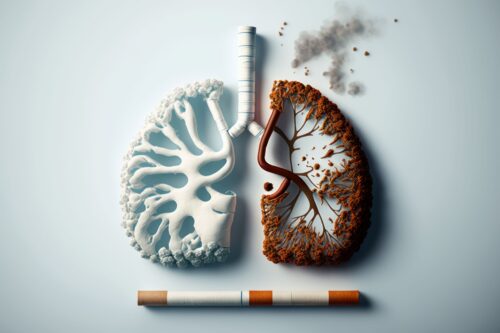
Breast cancer is a malignant tumor caused by uncontrolled division of breast cells. It not only damages healthy breast tissue but can also spread to lymph nodes, and even metastasize to the lungs, bones, and brain. When cancer cells severely impair organ function, organ failure may occur, ultimately threatening life.
Question 2: How common is breast cancer in Hong Kong?
Breast cancer is one of the most common cancers among women in Hong Kong. In 2022, there were 5,182 new cases, accounting for 28.6% of all female cancers. On average, 1 in 14 Hong Kong women may develop invasive breast cancer in her lifetime. It also ranks third among cancer-related deaths in women.
Question 3: Which age group is most affected?
The median age of diagnosis among Hong Kong women is 58, younger than in the U.S. and Australia. Over 90% of cases are aged 40 or above, yet the youngest case was under 20—showing breast cancer is not limited to older women.

Question 4: What is the survival rate of breast cancer? How are stages classified?
The survival rate is closely related to the stage at diagnosis: around 99% at stage I, but only 30% at stage IV. Early detection and treatment are therefore key to improving cure rates.
In Hong Kong, the staging system follows the internationally recognized TNM system, based on tumor size (T), regional lymph node status (N), and distant metastasis (M).
| Stage | Description |
|---|---|
| Stage 0 | Carcinoma in situ. Cancer cells remain in the ductal basement layer with no invasion—the earliest stage of breast cancer. |
| Stage I | Tumor ≤2 cm with no spread to axillary lymph nodes. |
| Stage II | Tumor >2 cm but ≤5 cm; or tumor <2 cm with cancer spread to 1–3 axillary lymph nodes. |
| Stage III | Tumor >5 cm with cancer spread to 4 or more axillary lymph nodes, or involvement of chest wall, skin, or supraclavicular lymph nodes. |
| Stage IV | Metastatic breast cancer, spread to distant organs such as liver, lungs, or bones. |
Question 5: Can breast hyperplasia develop into breast cancer?
Typical breast hyperplasia is a common benign change and does not become cancer. However, “atypical hyperplasia” carries a higher risk of breast cancer. Regular monitoring is recommended to lower risk.
Question 6: What causes breast cancer? Can it be prevented?
Many women think heredity is the main cause, but data from the Hong Kong Breast Cancer Registry shows that over 80% of breast cancer patients surveyed had no family history! Therefore, breast cancer is not solely determined by genetics. The exact causes remain unclear, but certain factors increase risk:
Non-modifiable risk factors
- Age: Risk increases with age.
- Family history: Having a mother, sister, or daughter with breast cancer.
- Genetics: Mutations such as BRCA are linked to higher risk.
- Reproductive history: Late first pregnancy, no children, or not breastfeeding increases risk.
- Menstrual and menopausal history: Early menarche or being overweight after menopause increases risk.
Modifiable risk factors
- Lifestyle: Lack of exercise, heavy drinking, smoking, unhealthy diet, obesity.
- Environmental factors: Night shifts, long-term chemical exposure (e.g., certain cosmetics, hair dyes, plastics) may increase risk.
While breast cancer cannot be fully prevented, the following measures help reduce risk:
- Maintain a healthy lifestyle: Balanced diet, regular exercise, weight control, no smoking or alcohol.
- Regular screening: Early detection of abnormalities, especially for high-risk women.
- Early treatment: Early-stage treatment has high success rates, reducing mortality significantly.
Lifestyle changes cannot completely eliminate risk, but healthy habits plus regular screening are key to reducing incidence and improving survival. You may use this breast cancer risk assessment tool to evaluate your risk.
Therefore, regular screening is essential—detecting subtle breast changes early minimizes impact. Book your health check now to protect yourself!

Question 7: How should breast screening be arranged by age group?
Breast screening should be based on age and risk factors. Early detection significantly improves cure rates.
| Age group | Recommended screening | Notes |
|---|---|---|
| Women aged 20–30 | – Breast self-exam – Ultrasound – Genetic testing |
Women under 30 generally have denser breast tissue. Radiation-based screening should be avoided, with radiation-free ultrasound preferred. For those with family history of breast or ovarian cancer, genetic testing is recommended to assess risk. |
| Age group | Recommended screening | Notes |
|---|---|---|
| Women aged 30–39 | – Breast self-exam – Ultrasound – MRI – Genetic testing |
Breast cancer risk gradually increases. Regular ultrasound is recommended. High-risk women or those concerned about breast health may add MRI and genetic testing for comprehensive risk assessment. |
| Age group | Recommended screening | Notes |
|---|---|---|
| Women aged 40 and above | – Breast self-exam – 3D mammography – Ultrasound – MRI – Genetic testing |
Breast cancer risk increases significantly. Annual 3D mammography is recommended. High-risk women or those concerned about breast health may add MRI and genetic testing for comprehensive risk assessment. |
Question 8: What are the differences between breast screening methods?
| Method | Description |
|---|---|
| Breast Ultrasound | Radiation-free, especially useful for assessing palpable lumps or dense breast tissue. Differentiates between cysts, fibroadenomas, and malignant tumors. |
| 3D Mammography | Detects subtle abnormalities, including non-palpable lumps and early microcalcifications. 3D imaging reduces tissue overlap, producing clearer, more accurate results. |
| Breast MRI | Radiation-free. Provides detailed internal breast structures. More sensitive than traditional methods, with sensitivity over 90%. Detects small lesions or lumps that mammography or ultrasound may miss. |
| Genetic testing | Blood test to detect mutations linked to hereditary cancers, including BRCA1, BRCA2, TP53, and PTEN. Suitable for those with family history. Only needed once in a lifetime. |
| Cancer marker CA 15-3 | A blood test measuring substances elevated by cancer. Levels may rise with cancer, but early disease often shows normal results. Not reliable for detecting early tumors or nodules. |

Question 9: How to correctly perform breast self-examination?
Breast self-examination is a basic screening method that helps detect abnormalities early. Recommended once a month for women aged 20 and above. For premenopausal women, perform on day 7–10 after menstruation starts. For postmenopausal women, choose the same day each month.
Steps:
1. Observe breast appearance
- Stand naturally in front of a mirror, observe breast size, shape, and skin color.
- Raise both arms, check for skin changes (dimpling, wrinkling, redness, swelling).
- Hands on hips, check for asymmetry.
2. Palpate the breast
- While lying down, place one hand behind your head. Use fingertips to examine the entire breast in circular motions, including the underarm area.
- Standing in the shower, use moist fingertips to check the breast in circular motions from outer edge to center.
3. Check nipple discharge
- Gently squeeze the nipple. Look for discharge that is bloody, clear, brown, or yellow-green.
- Spontaneous discharge from one nipple requires immediate medical attention.
If you notice lumps, skin dimpling (orange peel appearance), nipple retraction, abnormal discharge, or axillary lumps, seek professional medical advice promptly.
Beyond breast checks, women should not neglect general health screening, such as blood tests (liver and kidney function, cholesterol, blood sugar), pelvic ultrasound, and Pap smears—these help detect common health problems early.
*This article is for reference only. Please consult your doctor for professional medical advice.
References:
1. 醫院管理局. 十大癌症
2. 癌症基金會. 乳癌
3. 香港腫瘤學研究學會. 乳癌義診
4. 香港乳癌基金會. 定期乳檢
5. 香港乳癌基金會. 甚麼人容易患上乳癌?
6. 香港乳癌基金會. 1.3 怎樣看乳癌期數?
7. 衛生署. 乳癌
8. 衛生署. 2022年女性乳腺癌統計數字
9. Breastcancer.org. Breast Cancer Risk Factors
10. Hong Kong Breast Cancer Research Group. Breast cancer in Hong Kong, Southern China: the first population-based analysis of epidemiological characteristics, stage-specific, cancer-specific, and disease-free survival in breast cancer patients: 1997-2001.
11. The American of Breast Surgeons. Diagnostic and Screening Magnetic Resonance Imaging of the Breast
12. Susan G. Komen. Breast Cancer Screening for Women at Higher Risk